About Flat Foot
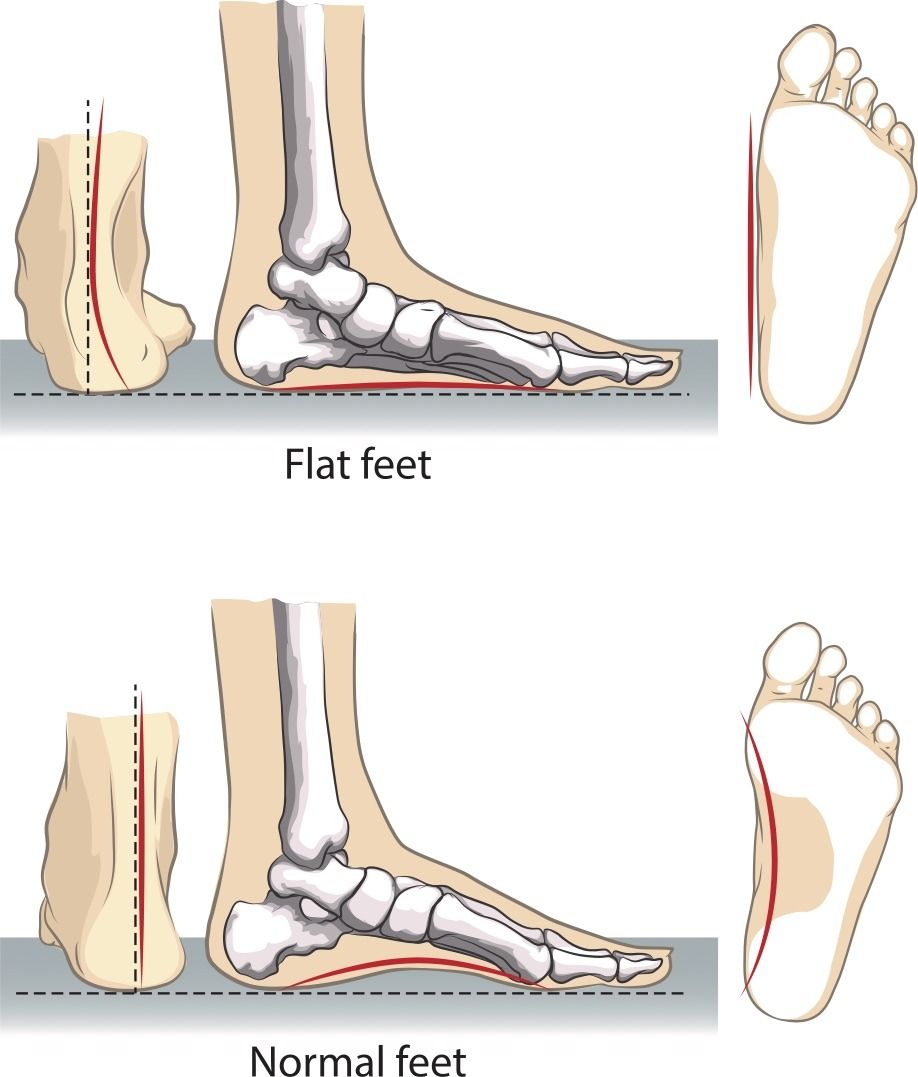
Flat foot – sometimes known as fallen arches – is a condition which is characterized by the absence of an arch, or upward curve, in the middle of the foot. This occurs when the tendons in the foot and lower leg fail to pull in unison to form this natural arch.
Causes
Flat foot has a number of potential causes. These include tendons which are torn or stretched; dislocated or broken bones; abnormalities which are present from birth; damage to the posterior tibial tendon which connects the middle of the foot arch to the ankle and lower leg; nerve problems; and certain health conditions, including rheumatoid arthritis.
There are several factors which are understood to increase the risk of having flat foot. These include old age, obesity, pregnancy and having diabetes.
Symptoms
The predominant feature of flat foot is the absence of an arch in the middle of the foot. In many cases, there are no problems which arise from flat foot, and thus there is no treatment required. However, other symptoms which do require attention may be experienced, such as achy and painful feet; inhibited foot movement; tired feet; swelling at the bottom of the feet; leg pain; and back pain.
Treatment
Before you are advised on a treatment path for flat foot, a diagnosis is typically made by a physical examination, and health history may also be checked for clues as to the cause of flat foot. A doctor can test the strength of the muscles in the feet and legs, and look for wear patterns on the soles of your shoes which may be unusual. Tests such as an MRI or x-ray can also be carried out.
The treatments which are recommended for flat foot will depend on the nature of the individual’s condition. Initial treatments can include stretching exercises designed to increase range of movement; physical exercises which can improve muscle strength; ice treatment and rest to address pain and swelling; shoe inserts; shoe modifications; and orthotic devices such as casts and braces.
Painkillers administered to relieve flat foot symptoms can include nonsteroidal anti-inflammatory drugs (NSAID) such as ibuprofen and naproxen. Injections of medications, including corticosteroids, can also be administered for the purpose of reducing inflammation.
For cases in which pain or damage to the foot is severe, surgery may be advised. Surgical procedures which are carried out to address flat foot can include excision, to remove bone spurs; arthrodesis, to fuse ankle and foot bones together; synovectomy, in order to clean the protective covering of the tendons; osteotomy, to cut the bone or change its shape; a lateral column lengthening, which involves the grafting of bone to the foot in order to improve the rise of the arch; and tendon transfer, which adds tendons from other parts of the body to the foot in order to help the tendons pull together and form the arch.