Plantar fasciitis
Plantar fasciitis is a common problem that causes pain under the heel bone often with lengthy walks and prolonged standing. It is most often seen in middle-aged men and women.
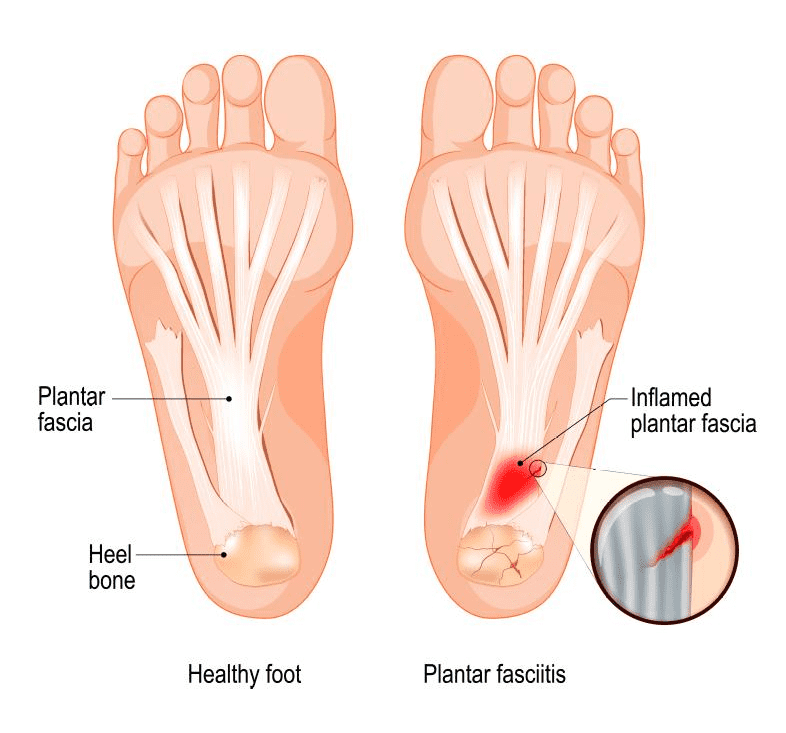
Plantar fascia is a thick band of tissue that lies at the bottom of the foot. It runs from the heel bone to the toe and forms the arch of the foot. The plantar fascia functions as a shock absorber and also supports the arch of the foot.
REQUEST AN APPOINTMENT
Causes
Too much of pressure over the fascia may damage or tear away the tissue and can be a cause of heel pain. It is also possible that when the plantar fascia gets overstretched or overused repeatedly, there may be irritation or inflammation of the fascia. Inflammation of the plantar fascia causes plantar fasciitis.
The risk factors that can make you more prone to develop plantar fasciitis include obesity, foot arch problems such as flat feet and high arch, activities such as long-distance running, ballet dancing and dance aerobics, occupations that necessitate walking or standing on hard surfaces for long period of time and wearing shoes with poor arch support or thin-soled shoes.
Symptoms
The most common symptom of plantar fasciitis is stabbing pain on the bottom of the foot near the heel. The pain develops gradually and may involve either one or both feet at the same time. Pain is usually worse in the morning or may aggravate after standing up for a long time.
Diagnosis
Your doctor will examine your foot and will check for the signs of flat feet or high arches, tenderness, swelling and redness of the foot and stiffness or tightness of the arch in the bottom of your foot.
Treatment
PRP (Platelet rich plasma)
New research has shown ultrasound guided PRP to have a therapeutic advantage when compared to steroid injection at one year follow up.
Most patients with plantar fasciitis are effectively treated with the following measures:
Medications
Your doctor may prescribe non steroidal anti-inflammatory drugs (NSAIDs) as they can reduce your pain and inflammation. Corticosteroids can be injected directly into the plantar fascia which may offer pain relief and reduce inflammation.
Rest
Decrease or avoid the activities that worsen the pain.
Ice
Apply ice pack over the painful area for at least twice a day for 10 – 15 minutes, for the first few days.
Night splints
Use of night splints is beneficial as it stretches the plantar fascia and allows it to heal.
Supportive shoes and orthotics
Your doctor may recommend you to wear shoes with good support and cushioning. Custom orthotics (shoe inserts) may also be helpful.
Physical therapy
Your physical therapist may suggest you an exercise program that focuses on stretching your plantar fascia and achilles tendon. These exercises may help to strengthen the muscles of lower leg. In addition to exercises application of athletic taping to support the bottom of your foot is also taught.
Extracorporeal shock wave therapy
During this procedure, sound waves are targeted to the painful area to stimulate the healing process in the damaged plantar fascia tissue.
Surgery
Rarely, surgery to release the tight plantar fascia may be needed. However it is recommended only after all nonsurgical measures have failed. Preventive measures such as stretching exercise programs and footwear modifications can help prevent plantar fasciitis.
As with all foot surgery it is normal for swelling to persist for some months after surgery and is completely normal. This swelling will eventually completely subside with time and can take up to 12 months but often goes well before this.
Ankle pain can be distressing, especially if you're not sure what options are open to you. If you're wondering if surgery could help you, book an appointment.
* Routine private appointments either face to face or remotely are available
