Insertional Achilles Tendinopathy
Insertional tendinopathy is a build-up of calcification within the Achilles tendon where it attaches into the heel. This causes a bony protrusion situated at the back of the heel bone. Insertional Achilles tendinopathy can quite often be painless, but in some cases, pain can be experienced at the back of the heel.
REQUEST AN APPOINTMENT
Causes
Insertional Achilles tendinopathy is sometimes associated with the plantar fasciitis condition; this typically occurs over a number of years as it can happen due to wear and tear of the Achilles tendon which connects the ball of the foot and the back of the heel bone. Plantar fasciitis typically produces painful symptoms.
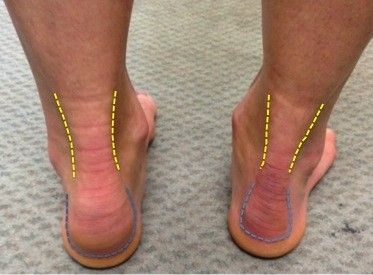
Risk factors associated with insertional Achilles tendinopathy include running on hard surfaces; walking gait abnormalities which exert excessive pressure on the heel bone, the heel ligaments and the nerves; obesity; and shoes which are badly worn, lack sufficient arch support, or are poorly fitted. It is also sometimes associated with a tight calf muscle.
Symptoms
It is common for insertional Achilles tendinopathy to cause no symptoms – but they can cause pain which is intermittent or chronic, which can occur when there is inflammation at the location of the spur formation, leading to a soft tissue injury. Symptoms can intensify with physical activities such as walking or running.
Insertional Achilles tendinopathy pain is characterised by a sharp stabbing sensation at the bottom of the feet, or a dull ache. It can often be experienced when first standing in the morning, or when standing for a prolonged period.
Treatment
Non-surgical treatment options for insertional Achilles tendinopathy can include stretching, strapping or taping allowing stressed muscles to rest, new shoes or shoes without a heel counter to press on the painful area, footwear with a slight heel raise, orthotic devices (shoe inserts), night splints, physical therapy, medications such as nonsteroidal anti-inflammatory drugs (NSAID) and paracetamol.
While in the vast majority of cases, insertional Achilles tendinopathy can be addressed with non-surgical treatments, in some cases a surgical procedure can be advised.
Surgery can be focused on the removal of a spur, detachment of the Achilles and reattachment using the SpeedBridge technique. Often a plaster cast is required for the first two weeks and then weight-bearing can commence in a boot with the foot pointing downwards. In can take three months to recover from this procedure, with swelling persisting for longer. A number of measures can be taken after the operation in order to aid recovery; these can include rest, ice treatment, elevation of the foot, and compression techniques.
As with all foot surgery it is normal for swelling to persist for some months after surgery and is completely normal. This swelling will eventually completely subside with time and can take up to 12 months but often goes well before this.
Ankle pain can be distressing, especially if you're not sure what options are open to you. If you're wondering if surgery could help you, book an appointment.
* Routine private appointments either face to face or remotely are available
