Ankle Instability
Are you fed up of ‘going over’ on your ankle? Perhaps you’ve been told that you have ‘weak ankles’? Maybe your ankle becomes painful or swells a little if you’ve played sport or been running? If so, you may have ankle instability.
Many patients will also describe their ankle as feeling ‘untrustworthy’ or that they favour one leg over the other. Ankle stability surgery can help get you back to being active.
REQUEST AN APPOINTMENT
Why do ankles become unstable?
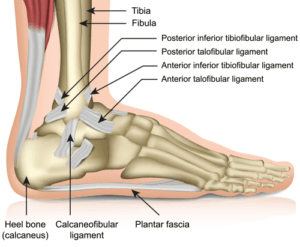
The ankle joint is much more than a hinge – together with the subtalar joint it allows the foot to move in three planes, and it needs to, in order for us to walk on uneven surfaces. A significant part of its structural stability comes from the ligaments that surround it.
On the inside (medial) part of the ankle joint, the is a big broad ligament called the deltoid ligament. On the outside (lateral) part of the ankle, instead of a single, broad, ligament, there are three individual ligaments (called the ‘ATFL’(anterior talofibular ligament), ‘CFL’(calcaneofibular ligament) and ‘PTFL’ (posterior talofibular ligament)).
A big proportion of ankle instability occurs because of tearing or stretching of these ligaments – particularly the lateral ligaments. Even a sprain from many years ago can have a knock-on effect, and sometimes, the little bit of instability within the ankle can create wear on the tendons (such as the peroneal tendons), which wrap around the ankle.
We now know that having an unstable ankle can also contribute to osteochondral lesions (cartilage damage) and ankle arthritis in the long-term.
Ankle instability surgery
At the end of the procedure, the incision will be closed with surgical staples or sutures. The ankle will then be bandaged before being placed in a splint. Following this period of recovery, you will usually need to wear a boot or cast. In general, you will need to avoid putting your weight on the affected ankle for anything from 2-6 weeks following the ankle fracture surgery procedure depending on your type of fracture and how strong your bone is. You will gradually begin to put more weight on the ankle as your recovery progresses. Resting and elevating your ankle will help with pain and swelling during your recovery.
You will normally be given a physical therapy programme with exercises designed to strengthen the ankle and improve its range of movement. Follow-up appointments involving an x-ray are scheduled to ensure your progress is on track.
Traditionally, surgeons have used a procedure called a Brostrom operation. This is a day case operation which is carried out under a general anaesthetic through a small incision, and the damaged ligaments are repaired or reattached to the ankle bones.
I prefer to carry out an operation which involves the Brostrum procedure plus the addition of what’s called an internal brace. This is a collagen coated fibretape which I attach to the talus bone at one end, and the fibula bone at the other end, and it sits on top of the repaired ligaments.
It acts as a mini ‘seat belt’, which protects the repair of the ankle ligaments whilst they are healing. This means that we can get you back to activity much faster.
I often check inside the ankle joint with an arthroscope (camera), to clear any soft tissue debris and to make sure that the surfaces are in good order.
How is ankle instability diagnosed?
When we meet, I’ll ask lots of questions about how your ankle behaves, what symptoms it’s giving you, what sports and activities you like to carry out, and whether there have been any previous injuries in the past.
I’ll examine how you walk, how your ankle moves, and whether there is some laxity when I stress it in certain directions.
I may ask you to undergo some tests such as X-rays and an MRI scan. This will help me understand if there has been any damage to the articular surfaces of the ankle, as a result of it being looser and what the current state of the ligaments are.
What are the treatment options for ankle instability?
Most patients with ankle instability will benefit from some physiotherapy to strengthen the ankle and retrain the ankle’s ‘proprioception’ (which helps the body’s balancing ability – a kind of movement correction if the ankle senses we’re about to wobble over).
Sometimes, if physio alone can’t help, it may be necessary to consider surgery, particularly if there has been extensive lateral ligament tearing. At the time of surgery, it may also be necessary to repair damage which may have occurred to the peroneal tendons, and have a look inside the ankle joint, to check on the integrity of the ankle joint’s cartilage surfaces.
What is the recovery like after instability surgery?
After your surgery, you’ll be in a plaster cast. This will stay on for two weeks, and I’ll ask you to get about on crutches, whilst resting as much as you can.
After two weeks, I’ll remove the cast and dressings, and you’ll be able to start gently weight bearing on your ankle, whilst wearing a supportive boot (which you can take off to wash and sleep).
At around six weeks, you’ll be able to get going with some physiotherapy or osteopathy to restore the movements in the ankle, and to strengthen the muscles. You can return to running at around three months, and by six months you’ll be able to fully return to contact sports.
It is rare for this kind of stabilisation to fail, and very occasionally a patient might end up with a little more stiffness in the ankle, but this is usually minimal and well tolerated.
Ankle pain can be distressing, especially if you're not sure what options are open to you. If you're wondering if surgery could help you, book an appointment.
* Routine private appointments either face to face or remotely are available

